- Reading time:
- 9 minutes
Share this post

What Is Healthcare Software Modernization (+ How to Start)
11 December 2025

Richard Katona
Head of Product Delivery
Healthcare software modernization isn’t just a tech upgrade but a way to enhance patient care, streamline operations, and ensure data security in an increasingly digital world. This guide walks you through what modernization means, why it matters, and how to approach it more confidently.

Quick summary
This article explains the challenges, strategies, and best practices for upgrading legacy systems safely. It highlights practical solutions and modern tools that help healthcare teams improve patient care without disruption. Check the Kodesage blog for more valuable articles on modernization and documentation.
Considering modernizing your healthcare software?
Many healthcare organizations still rely on legacy systems. These systems are important but often slow, hard to maintain, and costly to scale. Yet full replacements carry real risk, from compliance gaps to patient safety issues.
Healthcare software modernization offers a way forward. It helps teams improve performance and reliability without starting from scratch.
This Kodesage article breaks down what modernization means for healthcare software, the core challenges it solves, and how to approach it without breaking what already works.
What is healthcare software modernization?
Healthcare software modernization means upgrading outdated clinical systems so they are easier to maintain, safer to run, and ready to scale. These systems include electronic health records (EHRs), billing software, lab tools, and patient portals, many of which were built decades ago.
Modernization is not just a UI refresh or code rewrite. It involves improving four core layers:
- the underlying codebase and architecture
- the way data flows through systems and APIs (e.g. FHIR, HL7)
- the infrastructure (on-prem, cloud, or hybrid)
- the user experience for clinicians and administrators
Some of these systems still rely on aging stacks like COBOL or Visual Basic. Others use tightly coupled databases with no testing, no documentation, and no audit trails.
Why healthcare software needs modernization
- Operational inefficiencies and downtime: Legacy systems are slow, crash often, and are hard to troubleshoot. This delays patient flow, reduces clinician productivity, and creates backlogs.
- Poor interoperability and fragmented data: Outdated standards like HL7 v2 limit system communication. This creates data silos across labs, billing, and clinical apps, making it harder to get complete patient records.
- Compromised patient safety and data accuracy: Inaccurate or inaccessible data increases the risk of clinical errors. Legacy systems often lack validation, audit trails, and decision support, allowing small failures to escalate.
- Security and compliance vulnerabilities: Many older systems lack encryption, access controls, and role-based permissions. This raises the risk of HIPAA violations, breaches, and ransomware attacks.
- High maintenance costs and staff burnout: Legacy tech needs niche skills that are costly and rare. Patching and workarounds waste time, while poor workflows create repetitive manual work for clinical staff.
Examples of healthcare software that require modernization
Healthcare legacy systems are fragile and difficult to integrate with modern tools. Below are real examples of platforms that often need modernization due to performance, security, or interoperability limitations:
- EHR and EMR platforms: Many hospitals use on-premise EHRs that are difficult to scale and update. These often lack support for APIs, FHIR, or analytics.
- COBOL-based billing and finance tools: Large health networks still rely on COBOL systems for claims and payments, but skilled engineers are scarce, making updates challenging.
- Lab information systems (LIS): Older, custom-built LIS often lack documentation and API support, making integration with newer platforms difficult.
- HL7-only messaging systems: Many interfaces rely solely on HL7 v2 without FHIR or REST, slowing integration with telehealth and patient engagement apps.
- Government EHRs: Systems like VistA (VA) and AHLTA (DoD) are decades old and have faced modernization delays. In the UK, the NHS’s Lorenzo EHR has been replaced in parts for similar reasons.
Strategies for modernizing healthcare systems
1. Encapsulation: add new access layers without touching core code
Encapsulation involves wrapping legacy systems with modern APIs or service layers without changing the underlying code. This approach works well when core functionality is stable but inaccessible to newer platforms.
Healthcare teams often use encapsulation to expose HL7 interfaces or legacy business logic to external systems like patient portals or analytics dashboards. It’s a practical first step when deeper changes are too risky or constrained by regulatory requirements.
2. Rehosting: lift and shift to new infrastructure
Rehosting, often called lift-and-shift, means moving an application to a new infrastructure environment, typically from on-premise servers to private or hybrid cloud platforms, without altering the application itself.
This approach is useful when the application still performs adequately, but the hardware or hosting environment has become a liability. Many healthcare organizations use rehosting to reduce data center costs or improve system availability without the overhead of rewriting code.
3. Refactoring: improve the code without changing what it does
Refactoring focuses on improving the internal structure of an application without changing its external behavior. It’s ideal for legacy systems where the core functionality is still needed, but the codebase has become difficult to manage or maintain.
In healthcare, refactoring can reduce the risk of failure in high-use systems like scheduling platforms or lab interfaces, while extending their useful life. It includes simplifying complex modules, introducing automated tests, and improving code readability.
4. Rebuilding: rebuild the app from scratch using modern tools
Rebuilding is a full rewrite. It gives you control over architecture, workflows, and integration, but carries the most risk. This approach makes sense when legacy systems are no longer scalable, secure, or adaptable to changing requirements.
Rebuilding is often considered when legacy healthcare applications block the adoption of new care delivery models or patient engagement tools. While rebuilding requires the most time and resources, it provides full control over system design, compliance, and future integrations.
5. Replacing: swap legacy for a new off-the-shelf solution
Replacing involves decommissioning a legacy system and switching to a new vendor product or SaaS solution. It is best suited for cases where the existing system no longer provides strategic value and a modern alternative already exists.
Healthcare providers often choose this path for administrative tools like HR or billing platforms, where industry-standard solutions offer better support, lower costs, and easier integrations. The tradeoff is less customization and a need to adapt workflows to the new system.
6. Replatforming: move to a new platform with minimal changes
Replatforming involves migrating an application to a new platform, often to leverage better performance, scalability, or security, while making only minimal code changes. This approach keeps the core functionality intact but allows teams to take advantage of new infrastructure capabilities.
In healthcare, replatforming might involve moving from an on-premise database to a HIPAA-compliant cloud service. This can improve reliability and enable integrations with modern analytics or patient engagement tools, all without a full rebuild.
7. Retiring: phase out outdated systems and consolidate functions
Retiring means decommissioning systems that no longer provide value and consolidating their functions into other platforms. It’s an effective way to reduce operational complexity, cut costs, and free resources for modernization efforts that matter most.
Healthcare organizations often retire outdated reporting tools, data repositories, or departmental applications that have been replaced by more capable, centralized systems. This reduces security risks from maintaining unused or unsupported software.
8. Phased modernization: update in smaller, manageable steps
Phased modernization breaks a large modernization effort into smaller, sequential updates. This approach reduces risk, limits downtime, and allows teams to learn from each stage before moving to the next.
In healthcare, phased modernization might mean upgrading the patient records system in stages, first improving the database, then introducing new APIs, and finally rolling out a modern user interface. This ensures critical services remain available while still moving toward a fully modernized system.
How tools and platforms aid healthcare software modernization
Modernizing healthcare systems is about understanding what exists, where the risks are, and how to change systems safely.
Tools that support modernization help teams decode legacy systems by offering:
- System visibility: Dependency mapping and architectural overviews make it easier to spot bottlenecks and fragile areas.
- Documentation support: Automated documentation tools reduce reliance on tribal knowledge and speed up onboarding.
- Standards alignment: Integration with HL7, FHIR, and other clinical standards ensures smoother interoperability.
These platforms make it possible to layer new APIs, secure data flows, and extend legacy capabilities, without having to start from scratch.
How Kodesage supports healthcare software modernization
Kodesage is built for engineering teams working on high-stakes, undocumented systems that are difficult to scale or modify. Here’s how it supports healthcare software modernization.
A unified knowledge engine for legacy systems
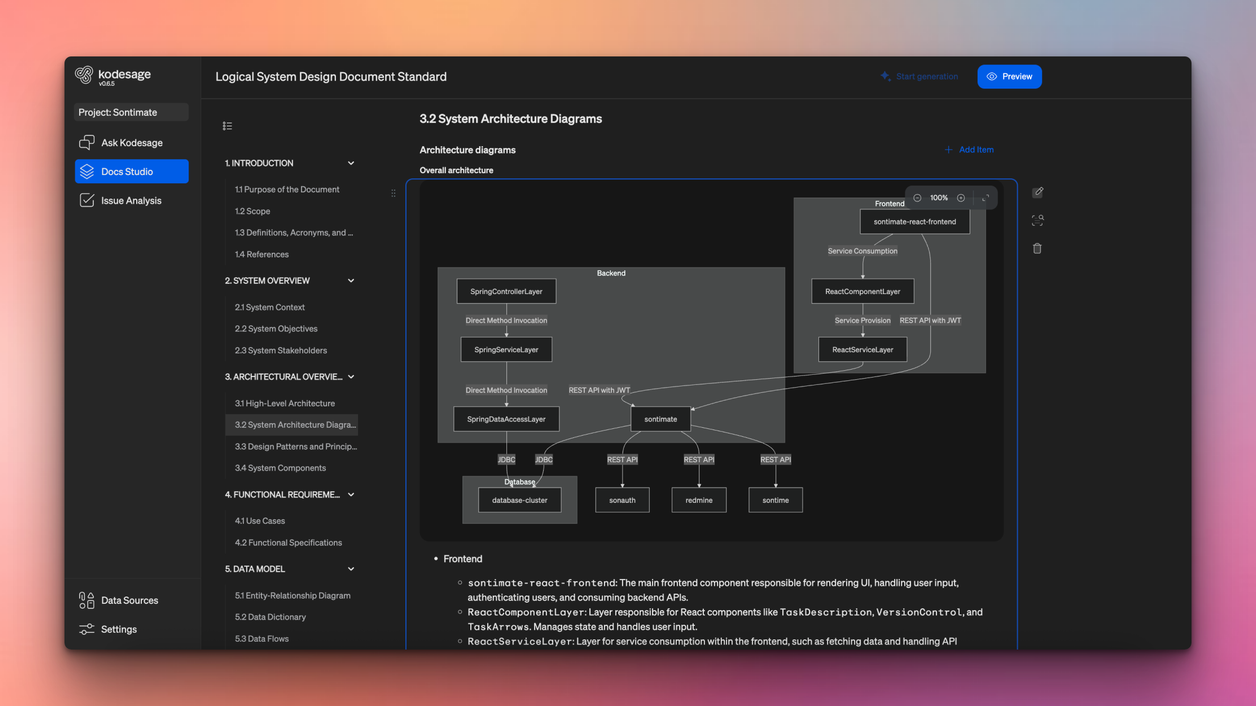
Instead of relying on isolated documentation or brittle tools for legacy system modernization, Kodesage creates a unified view of technical knowledge, spanning codebases, databases, tickets, and more.
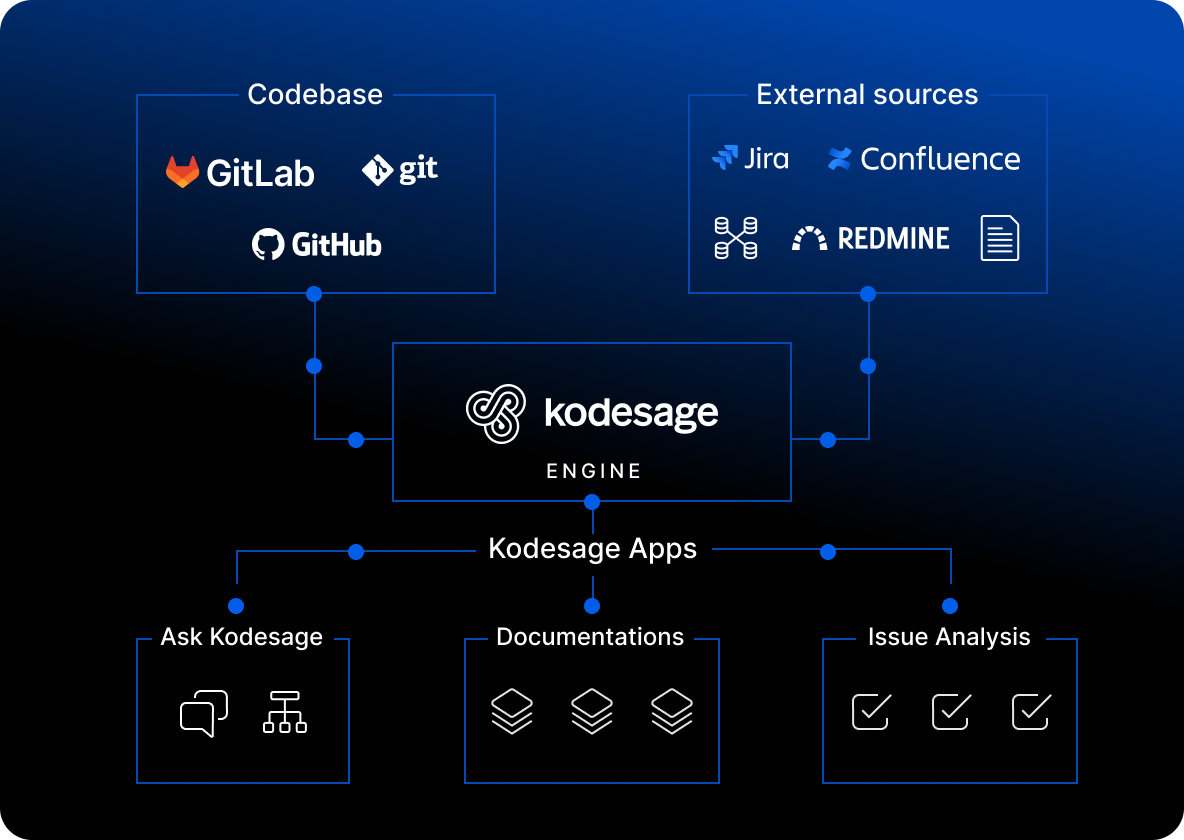
This dynamic knowledge base maps relationships across APIs, services, and business logic, enabling:
- Semantic code search for faster understanding
- Auto-generated documentation that stays in sync
- LLM queries for context-aware insights
Developer workflows made easier
Through it's API and IDE integration, Kodesage:
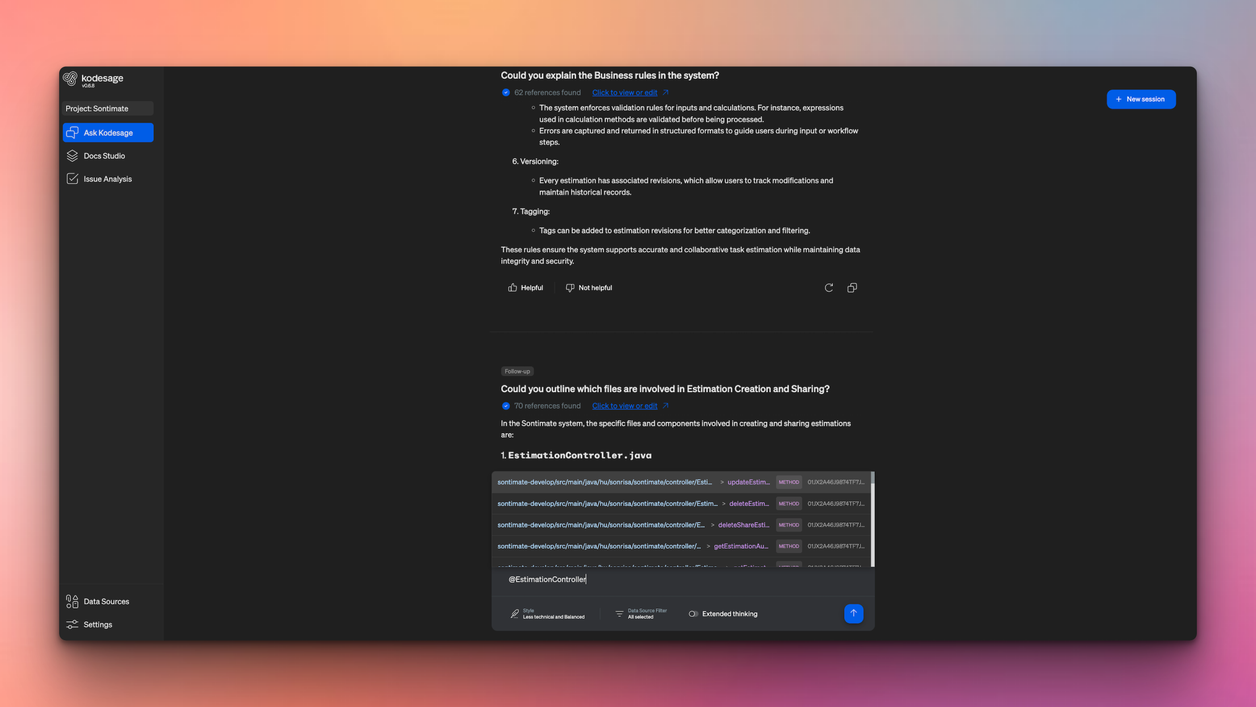
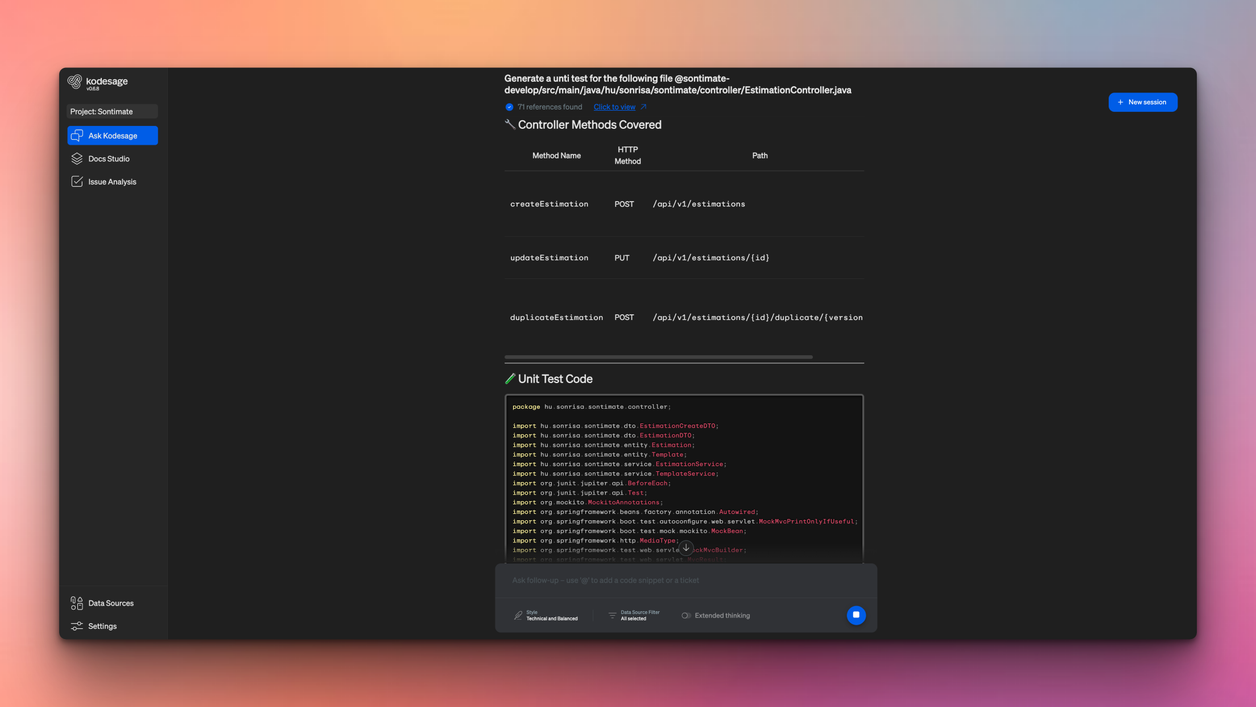
- Offers natural language Q&A via “Ask Kodesage”
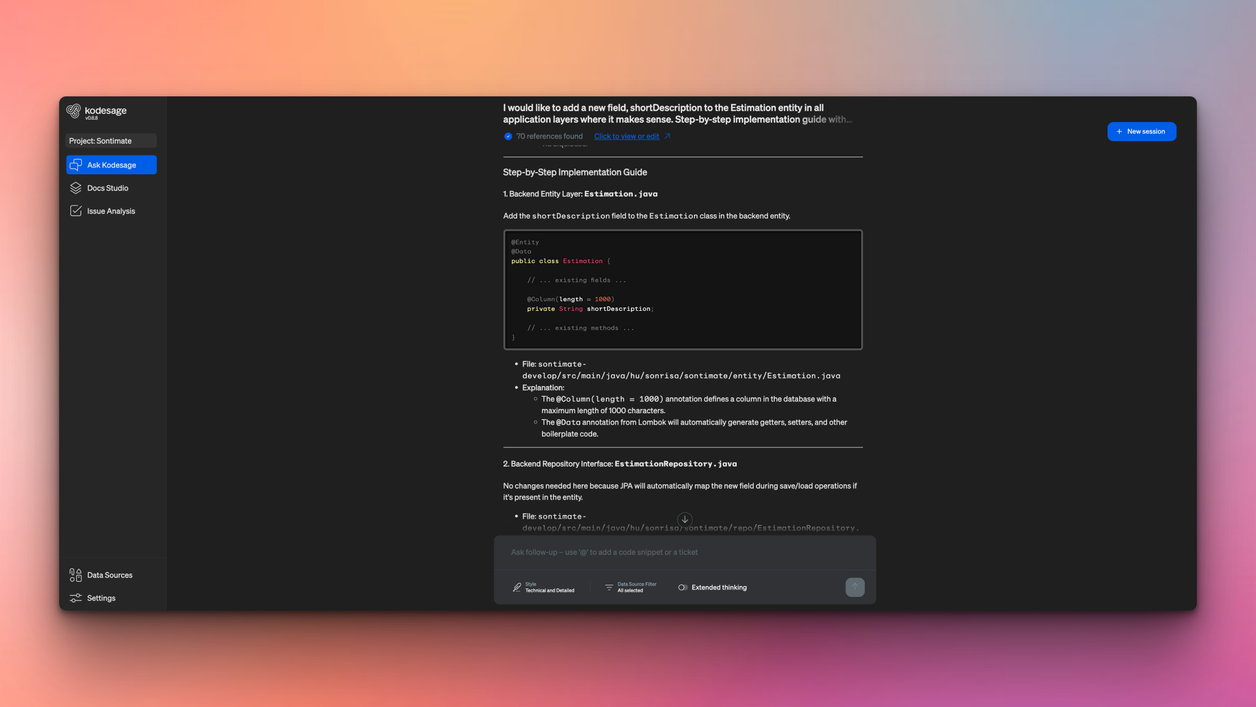
- Provides instant context for safer code changes
- Provides implementation plans and detailed guides
Increase production support efficiency
By integrating with issue ticketing systems, and having legacy languages specific parsers, Kodesage supports:
- Support teams by providing automating fix suggestions for issue tickets
- QA teams by automating unit and regression test generation
- Product managers and business analysts with faster discovery
Kodesage is not just a documentation tool. It is a modernization companion built to reduce risk and accelerate progress on even the oldest systems.
Challenges of healthcare software modernization
- Fragmented systems and data silos: Different vendors and departments use incompatible systems, creating duplicated records, broken workflows, and inconsistent patient data.
- Outdated tech stacks and architectures: Many systems run on COBOL, Visual Basic, or undocumented custom monoliths. These are hard to scale and difficult to test, forcing teams to spend more time decoding than improving.
- Compliance, privacy, and security constraints: Strict regulations like HIPAA make changes high-stakes. Many legacy systems lack access controls, encryption, and audit trails, putting patient data at risk.
- Clinician adoption and resistance to change: Clinicians may resist new tools if they’re used to existing systems. Poor UX or lack of trust reduces adoption, leading users to stick to old workflows.
- Migration risk and operational downtime: Critical platforms can’t go offline without affecting care. Large rewrites or rushed migrations raise the risk of failure, making incremental changes safer.
- Cost, ROI, and stakeholder alignment: Modernization requires investment in tools, infrastructure, and training. Without clear ROI or alignment between IT, clinical, and leadership teams, projects stall.
Best practices for healthcare software modernization
Successful healthcare modernization balances innovation with patient safety and compliance. Use these best practices to guide your project and reduce risks.
Conduct a comprehensive system audit
Start by evaluating your current systems to uncover performance issues, security gaps, and documentation needs. This baseline helps you set priorities and allocate resources effectively. AI-powered legacy knowledge platforms like Kodesage can accelerate this process by scanning centire codebases, mapping dependencies, and automatically generating up-to-date documentation.
Prioritize user-centric design
Engage clinicians, nurses, and administrative staff early in the process. Their input ensures the system supports real workflows, reduces friction, and improves usability, which leads to higher adoption rates and better patient care.
Implement modular architecture
Build systems in modular parts to allow incremental updates and easier integration without disrupting the whole platform. This approach enables incremental modernization, faster integration of new features, and less disruption to critical healthcare services.
Ensure robust data governance
Establish clear policies for data quality, privacy, and compliance with healthcare regulations such as HIPAA. Strong governance maintains trust, supports interoperability, and ensures the system remains audit-ready.
Adopt agile development practices
Use flexible methods that enable continuous improvements and quick adaptation to changing healthcare needs. Agile cycles make it easier to deliver value faster while managing risk.
Modernize healthcare software using Kodesage
Healthcare software modernization is essential for improving patient care, ensuring data security, and meeting evolving compliance requirements. Outdated systems limit efficiency, increase operational risk, and make it harder to deliver quality outcomes.
Kodesage empowers healthcare teams with AI-driven system visibility, semantic search, and automated documentation to simplify complex modernization projects. It connects code, tickets, and schemas into a unified knowledge base that accelerates safe updates.
Book a demo to see how Kodesage can help your team modernize legacy healthcare systems confidently.
Why choose Kodesage?

Deep Legacy Code Intelligence
Kodesage supports legacy stacks like Oracle Forms, COBOL, PowerBuilder, SAP, PL/SQL, and also modern stacks.

Secure On-premise Deployment
Single tenant application, offering both VPC and fully on-premise deployments meeting the strictest security requirements.

Living Knowledge Base
Connect to the entire codebase, issue ticketing systems like Jira, databases, tests, wikis like Confluence and upload documents.

Automated Documentation
AI generated software documentation that is always up to date with a pre-built and editable document template library.

Regression Test Automation
Automate regression and unit test coverage, accelerate releases and ensure traceability for future audits.

AI-powered Issue Ticket Analysis
Native integration to systems like Jira, and AI-generated fix recommendations for tickets.
Start transforming your legacy systems
With Kodesage teams maintain legacy projects more efficiently, and modernize faster.
See it in action today.